Overturn Improper Downgrades and Denials Automatically
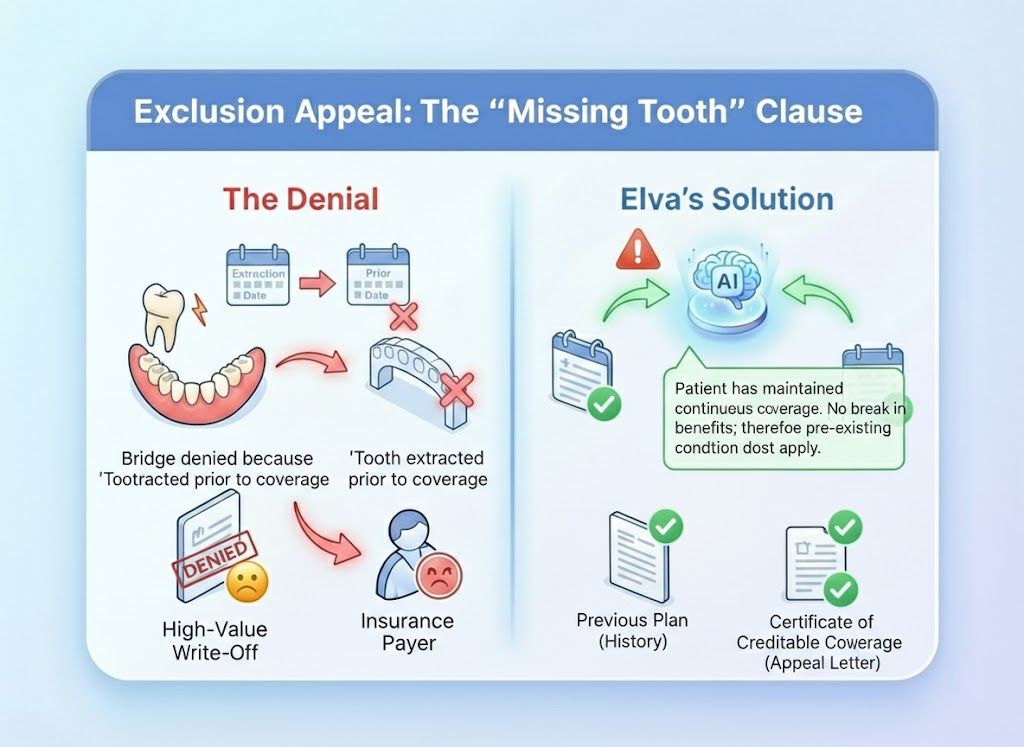
Payers use automated algorithms to deny or downgrade 30% of valid claims. Elva fights back with equal force. It instantly reads denial codes (CARC/RARC), cross-references them with clinical evidence, and writes irrefutable, data-backed appeal letters that recover the revenue you’ve already earned.
Code Interpreter
Translates cryptic denial codes (like "CO-45" or "Missing Info") into plain English instructions for your team.
Auto-Appeal Writer
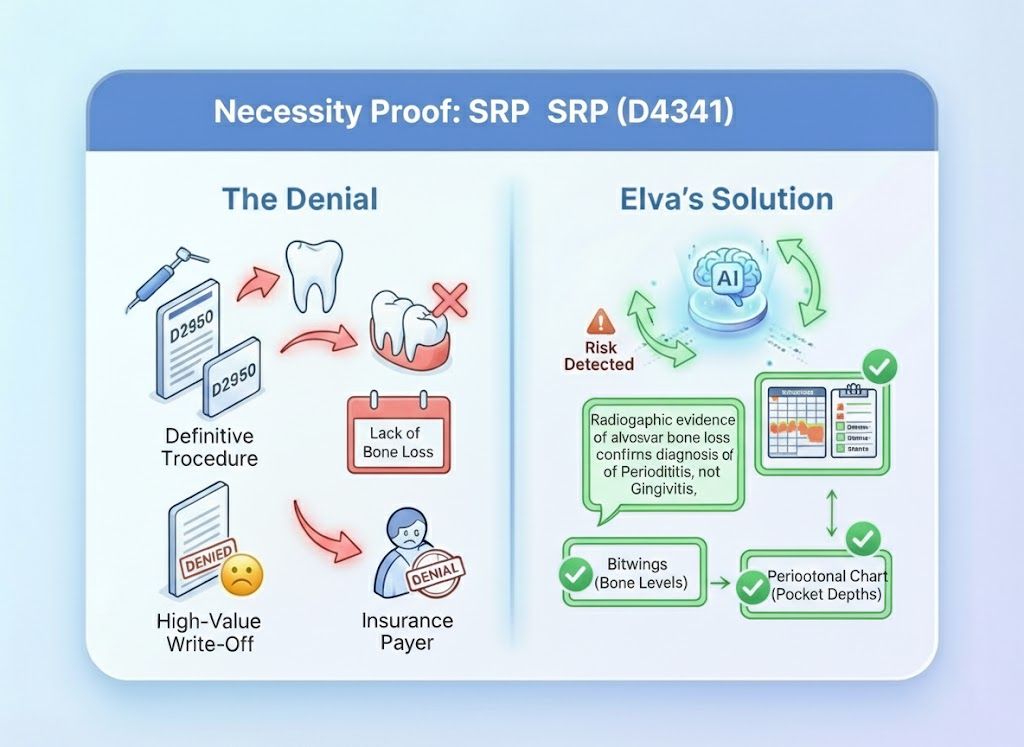
Generates professional appeal letters citing specific clinical findings (e.g., "50% bone loss") to reverse "Medical Necessity" denials.
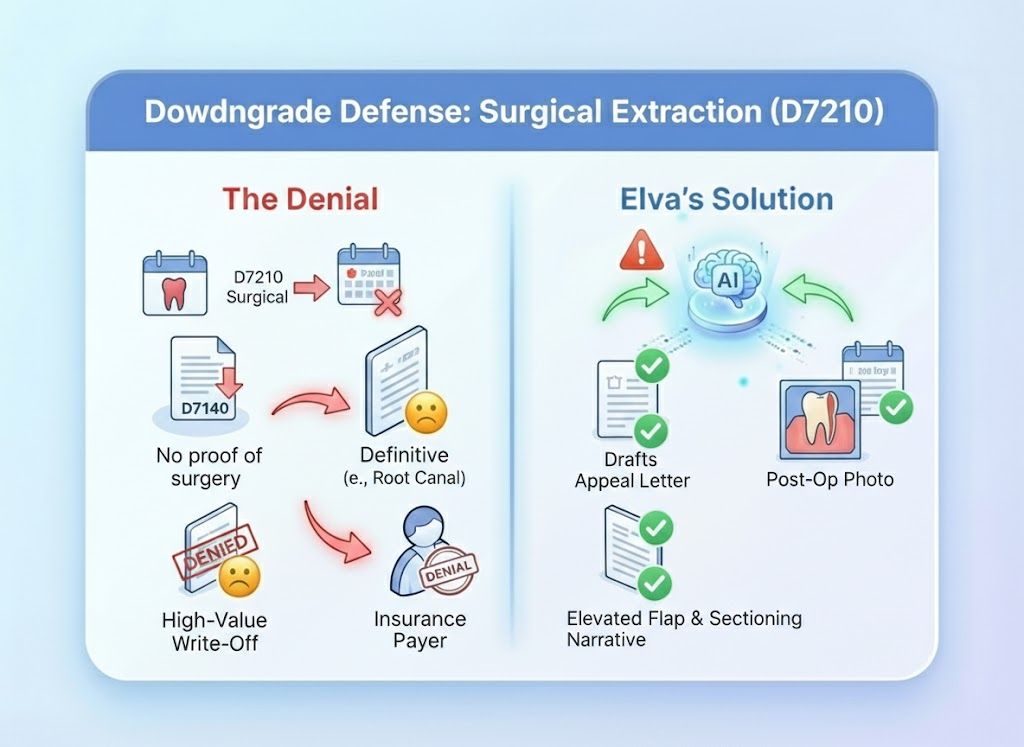
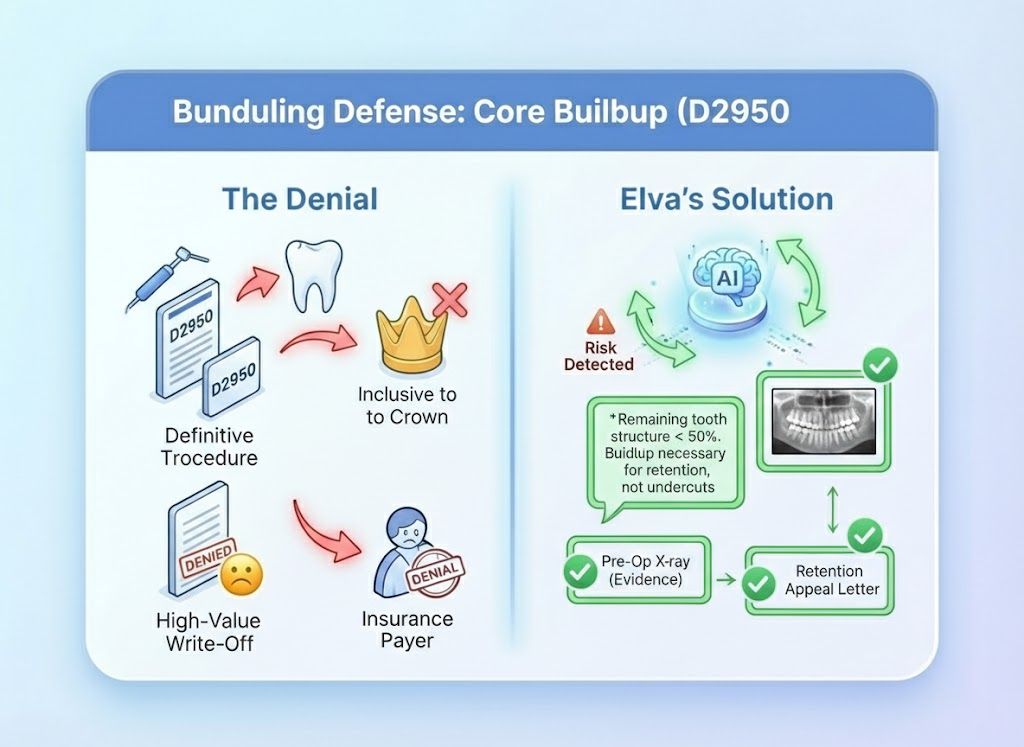
Downgrade Defense
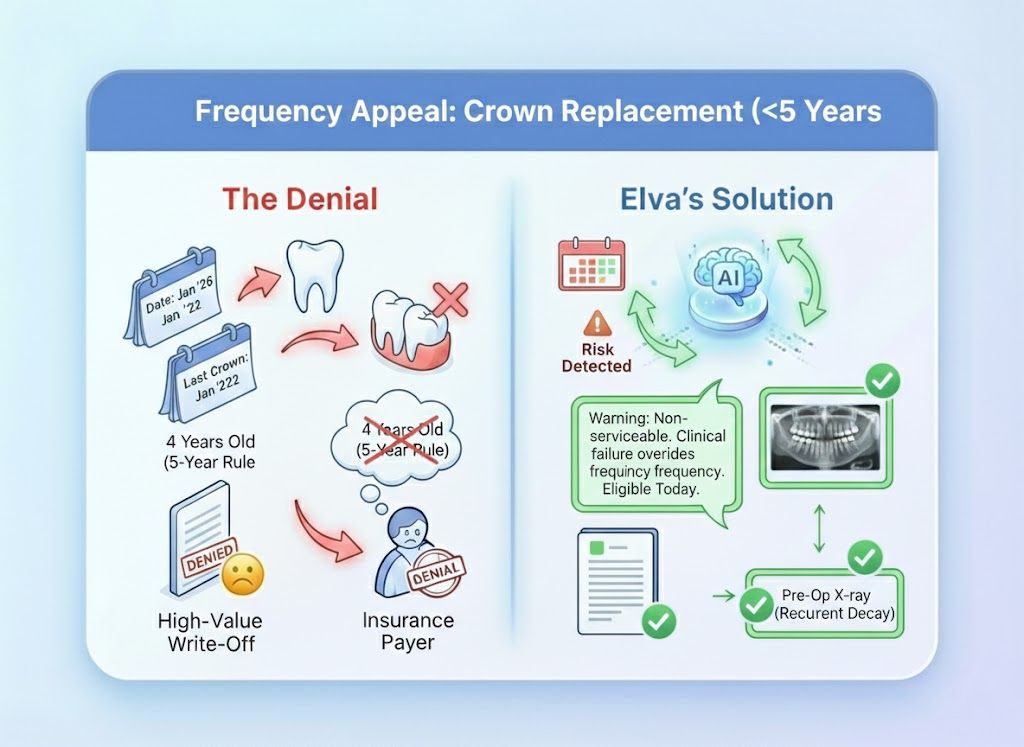
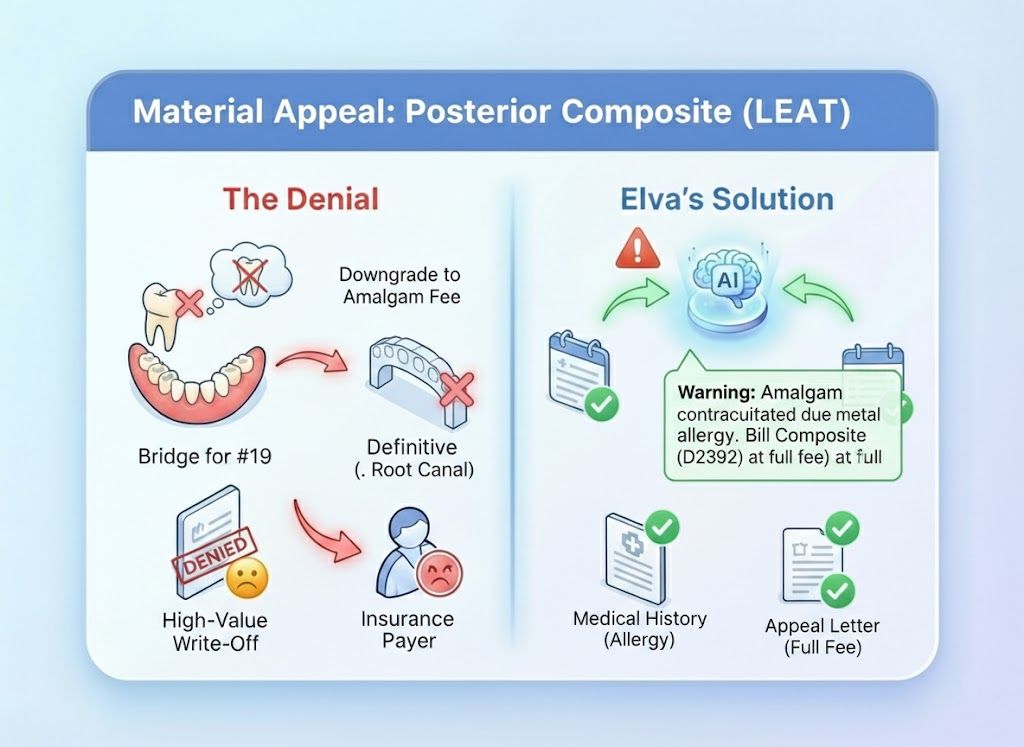
Identifies when a "Least Expensive Alternative Treatment" (LEAT) clause was applied and calculates if an appeal is viable.
Timely Filing Watchdog
Tracks the appeal window for every rejected claim, ensuring you never miss the deadline to fight for payment
The "Write-Off" vs. The "Fight Back"
The Old Way (Spreadsheet Purgatory): You get a stack of EOBs. You highlight the denials, put them in a folder, and plan to "get to them Friday." Friday never comes. You eventually write off thousands of dollars because you didn't have time to find the X-rays and write the letters. The Elva Way (Instant Rebuttal): Elva sees the denial the moment the ERA lands. It pulls the X-ray, highlights the pathology, drafts the appeal letter, and puts it in your "Ready to Send" queue. You recover revenue while you sleep.

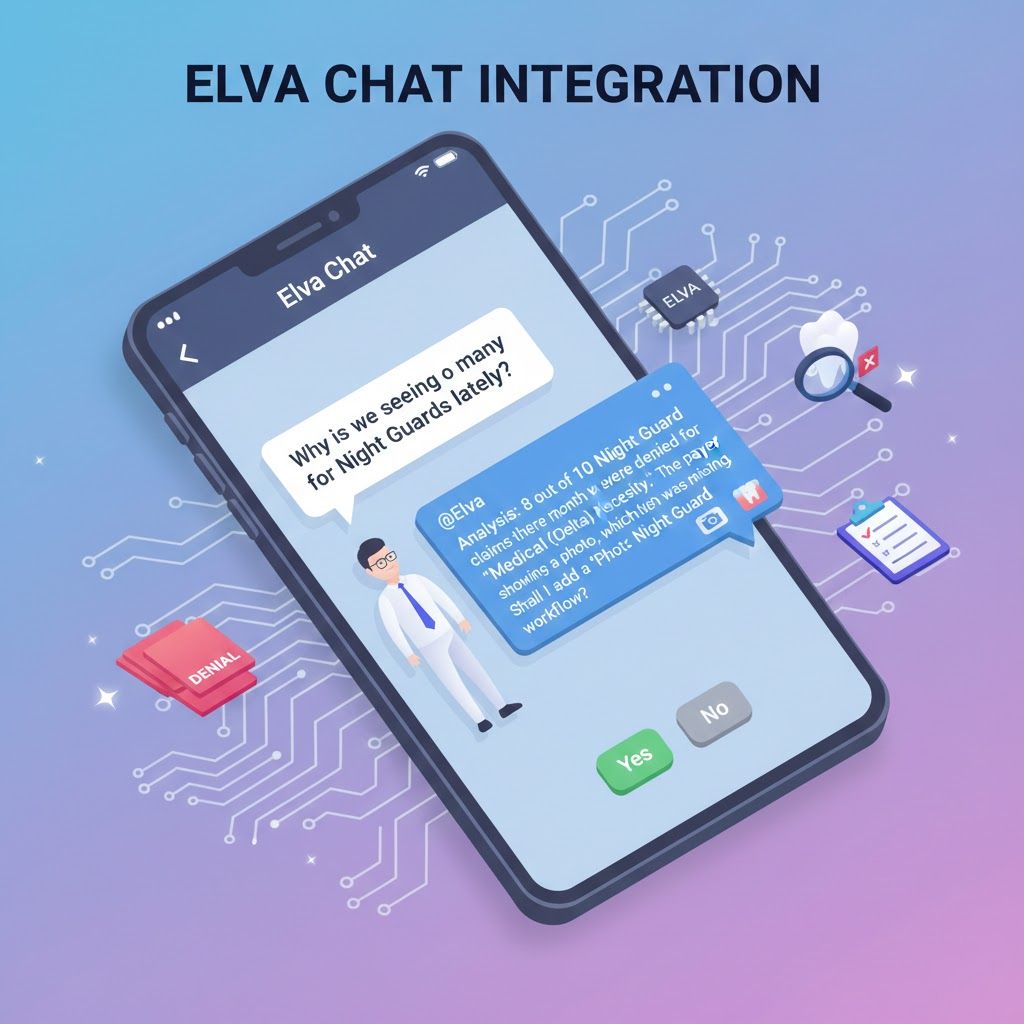
Don't hunt through the mail. Just ask.
our team can ask Elva to analyze denial trends or specific cases instantly. Office Manager: "Why are we seeing so many denials for Night Guards lately?" @Elva: "Analysis: 8 out of 10 Night Guard claims this month were denied for 'Medical Necessity.' The payer (Delta) requires a photo showing wear facets, which was missing. Shall I add a 'Photo Required' rule to the Night Guard workflow?"
The "Rubber Stamp" Denial Ends Here
Insurers bet that you are too busy to appeal a $150 denial. Elva isn't. It systematically challenges every improper adjustment, turning "Write-Offs" back into "Revenue."
The Automated Recovery Unit
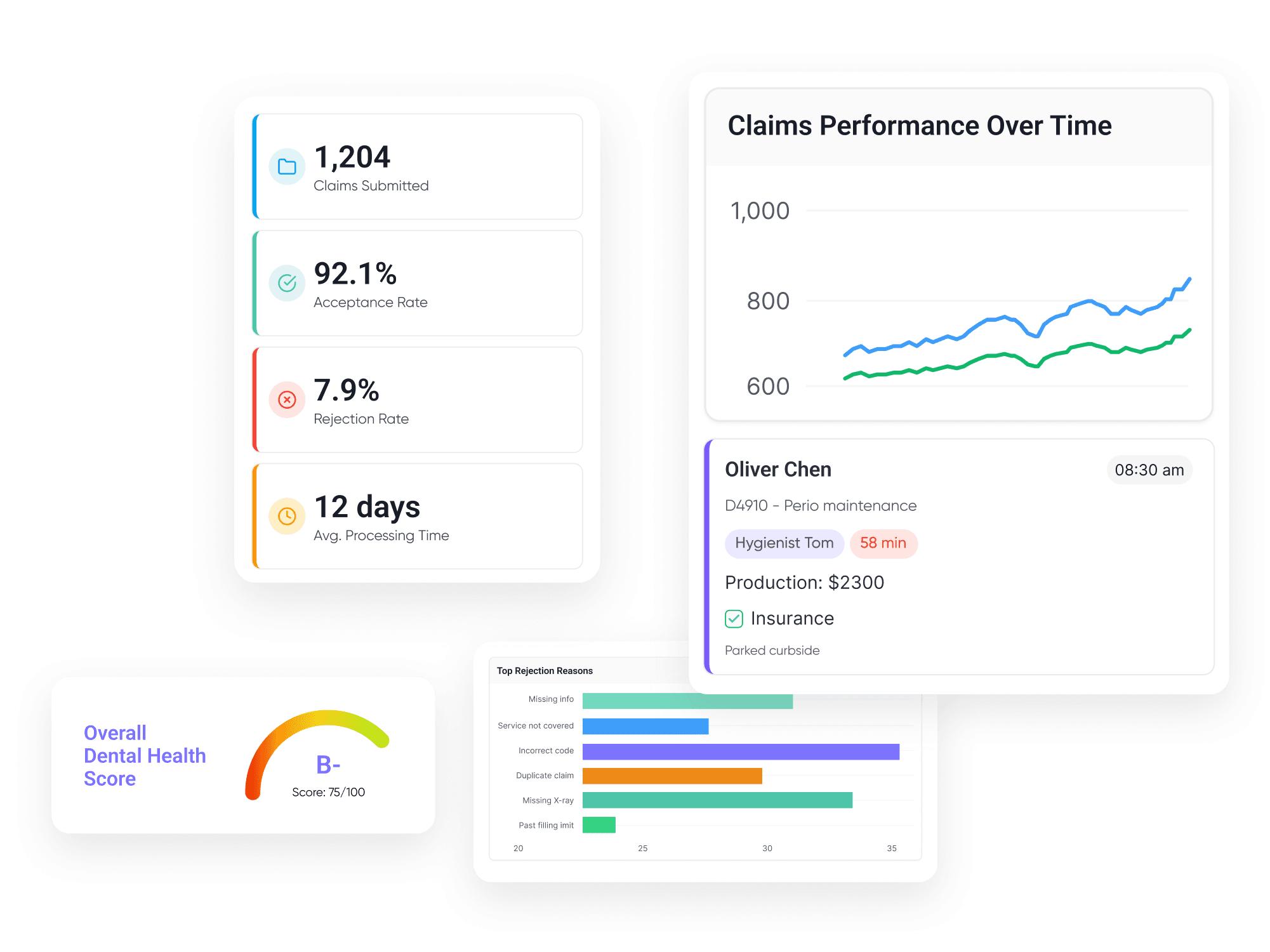
Elva turns "Denials Management" from a chaotic pile of paper into a streamlined digital workflow.

ERA/EOB Autopsy
"At-Risk" Revenue Dashboard

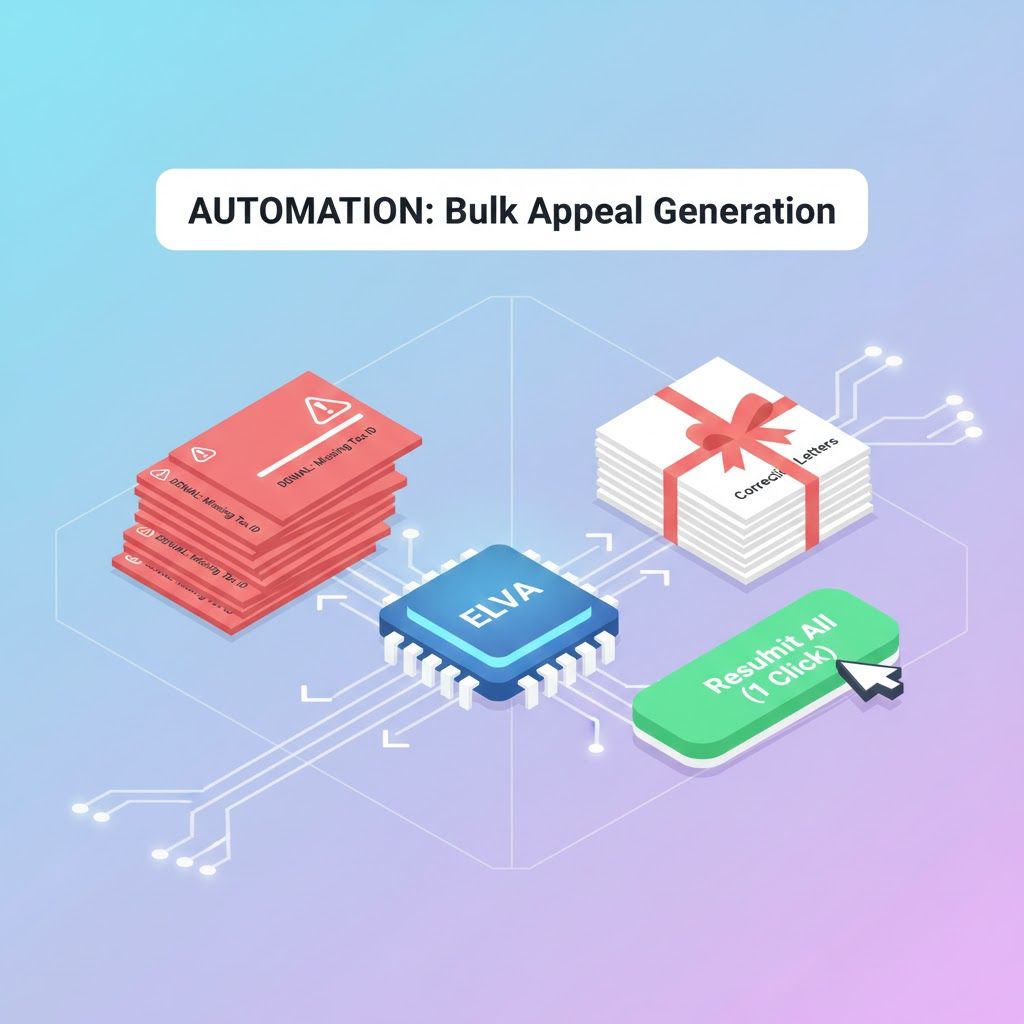
Bulk Appeal Generation

Root Cause Analytics
The "Reversal" Logic Layer
Elva knows the specific clinical keywords that adjudicators are legally required to accept. It builds the argument for you.
Fight Every Wrongful Denial
Don't let insurance companies keep your money. Equip your team with the AI that fights every denial with clinical precision.
Schedule a Demo